SAN MATEO — As cases of Mpox rise abroad, residents in San Mateo County still face barriers to getting vaccinated.
This low uptake comes as a more severe strain of Mpox, Clade IB, surges in the Congo with first confirmed spreading to Germany and the UK last week. There are no reports of any Clade IB cases in the US, yet.
The CDC recommends vaccination for men who have sex with men and are at increased risk of transmission. Jynneos, the Mpox vaccine which is a two-dose series, has been found to be 80% effective in preventing infection. It works both against Clade IB, and Clade 2B which dominated the 2022 outbreak.
Vaccination rates in the counties surrounding San Francisco are lower than those of California’s major cities.
“MPOX vaccine uptake has been greatest specifically in LA and San Francisco… the rest of the state has struggled,” says Vivian Levy, director of Infectious Disease in San Mateo County. “STI budgets nationally [and] statewide have really focused on urban centers.”
She has witnessed firsthand the difficulties patients in rural and suburban areas can face in trying to get vaccine access. Levy says that some San Mateo residents have needed to go into San Francisco to get vaccinated.
“We’ve heard from patients that it is not easy to find the MPOX vaccine,” says Levy. “And I’m still seeing among the [2B] cases, quite a bit of unvaccinated.”
This difficulty in access is not necessarily due to a vaccine shortage, but rather insurance issues and cost. While the vaccine was originally free during the 2022 outbreak, on April 1, Bavarian Nordic A/S, the vaccine manufacturer, made the vaccine commercially available instead. It is currently $270 per dose for private purchase.
“That creates a runaround and opportunities for people to fall through the cracks,” says Stephanie Cohen, director of HIV and STD Prevention at the San Francisco Department of Public Health.
People may now go to their pharmacies and find out that their insurance does not cover the vaccine or there is a fee attached which could deter uptake, according to Cohen. Coverage is not federally required until Jan. 1, 2025.
While health departments, like the SF Department of Public Health and the San Mateo Department of Public Health also buy stocks of vaccine to cover uninsured patients, there can still be issues with getting the information out about how to get an affordable vaccine.
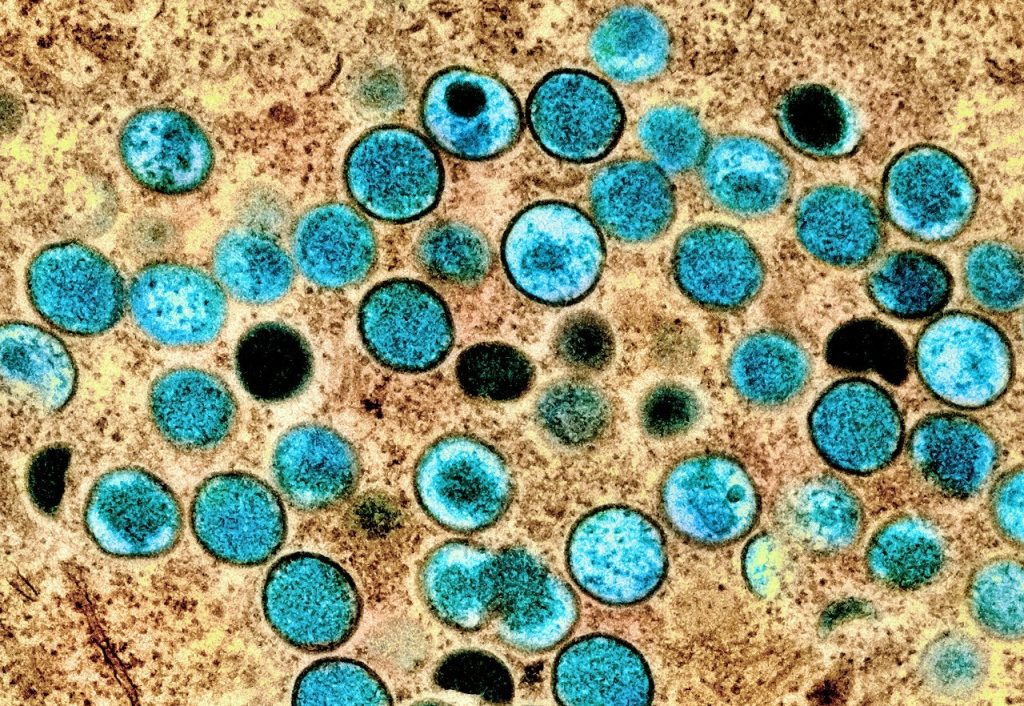
Mpox, formerly known as Monkeypox, is a virus that causes a painful rash or lesions in addition to flu-like symptoms. More severe symptoms can follow in some cases. Clade 1B has been seen to spread through household contacts, primarily affecting children in the Congo. This Clade can also spread through sexual contact. Clade IB has increased transmission and has caused more deaths than Clade 2B. Clade 2B which was prominent during the 2022 outbreak spreads mostly through sexual contact in men who have sex with men. Clade 2B is still circulating at low levels in the US.
There is also added concern for the Latino community in the US. During the 2022 outbreak, Latino communities had disproportionately high case rates. This is due to a variety of factors such as stigma, healthcare access, insurance status, and other social determinants of health, according to Cohen.
“We know that some sexual networks are racially segregated. So once an STI enters a network, that’s predominantly, composed of one racial ethnic group they may spread more quickly throughout that population,” she says.
Levy echoes these sentiments with her experiences in San Mateo County.
“Unfortunately, the populations that are left behind are not populations that have historically advocated for themselves… recent immigrants may not be able to navigate advocating for themselves in health systems that well, says Levy.
She is especially worried about vaccination for recent immigrants who fall into at risk populations but may not be publicly out to their communities. More needs to be done for both patient and provider education regarding Mpox, according to Levy.
This lack of education includes reduced focus on preventative measures.
“It’s kind of hard to get a lot of health systems engaged in kind of rolling out system wide things like mpox vaccine when you don’t have any active cases… and then when that pressing need comes up then all of a sudden all of these gaps start to really kind of show up,” says Frank Trinh, chief of staff of San Mateo medical center and medical director of mobile clinics.

